
In many cases, treatment for a junctional rhythm depends on the cause. The vagus nerve is the longest of your 12 cranial nerves and is associated with the function of many other organs, too.

This form of suctioning, known as endotracheal suctioning, can trigger vasovagal stimulation. lithium (Priadel, Camcolit, Liskonium, Li-Liquid)Ĭhest trauma and any injuries that require mechanical ventilation using suctioning movements deep in your throat can trigger junctional tachycardia.Several types of medications can also trigger a junctional rhythm, including: Some common medical causes of junctional rhythms include conditions like: There are a number of medical conditions, injuries, and even medications that could cause you to develop this abnormal heart rhythm. Each represents conduction that though slowed, is still ongoing through the AV node, and His-Purkinje system, respectively.What are the most common causes of junctional tachycardia? First degree AV block and intraventricular conduction block can occur independently of one another, or together. This is sometimes called aberrantĬonduction or intraventricular conduction delay, or it may be described by the characteristic appearance of a right or left bundle-branch block. This results in longer time required to completely depolarize the ventricles and is expressed in a prolonged (wider) QRS. When a portion of the His–Purkinje system fails to conduct (as in bundle-branch block) or conducts too slowly, the portion of the heart to which it extends is excited instead by muscle-to-muscle conduction.
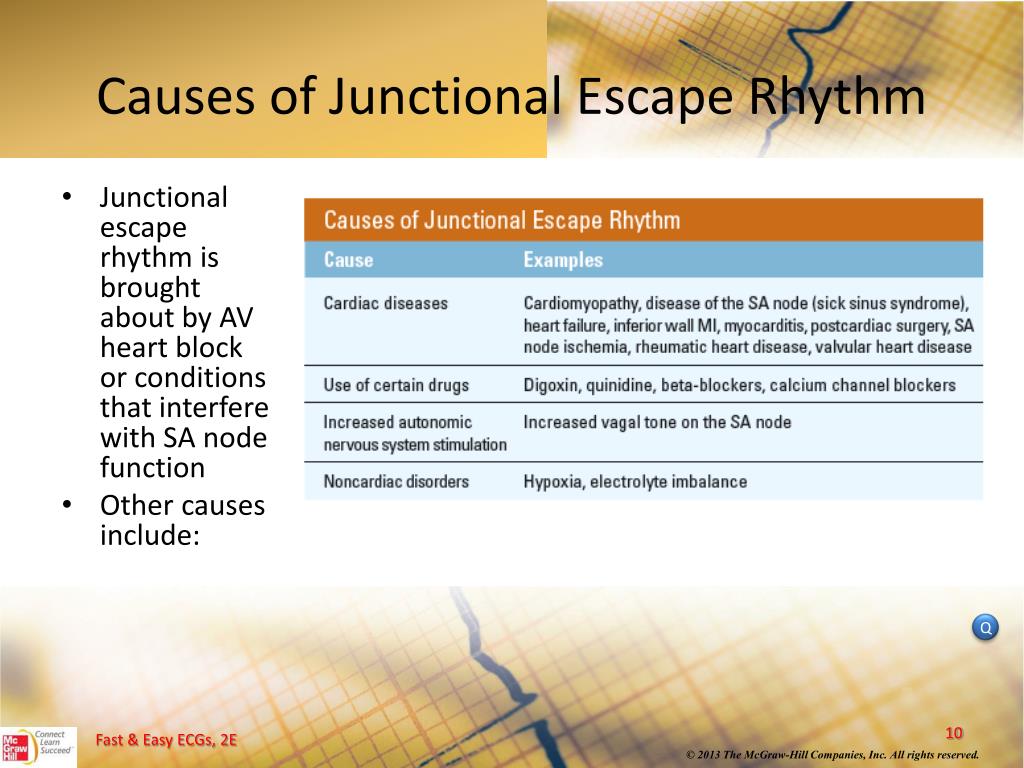
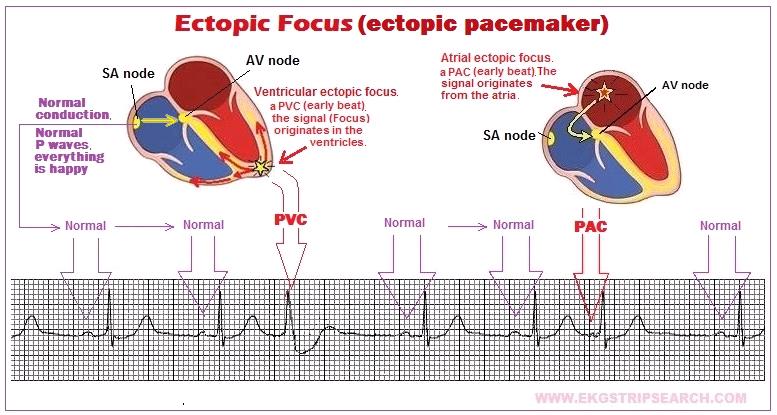
This is because conduction via the His–Purkinje system is much faster than conduction of an electrical impulse from muscle to muscle. Similarly, a slowing or partial block of conduction in the His–Purkinje system (as exemplified by bundle-branchīlock) results in a lengthening of the time required to completely depolarize the ventricles. The less common cause is due to slowing of conduction in the bundle of His. The most common location of such slowing is in the AV node. Should impulse formation fail at higher levels, the activity of these otherwise suppressed automatic sites may become manifest.įirst-degree AV block is defined as prolongation of the PR interval (the onset of the surface P wave to the onset of the QRS complex) to >0.20 second ( Fig. Impulse formation in junctional automatic tissue, for example, typically occurs at a rate of 40 to 60 beat per minute (bpm) His automaticity at a rate of 40 bpm and ventricular automaticity at 30 to 40 bpm. In addition to the sinus node, automatic tissues in other portions of the heart serve as subsidiary pacemakers, which can take control of impulse formation should the sinus node fail, but at a slower rate. Phase 4 of the action potential is heavily dependent on autonomic tone, with parasympathetic (vagal) tone typically slowing impulse formation and sympathetic tone accelerating it. Impulse formation originates in specialized tissue in the sinus node and is dependent on phase 4 (spontaneous depolarization) of the action potential. If either of these fails, an escape rhythm (originating from a subsidiary site of impulse formation) can serve as a backup pacemaker. The normal cardiac rhythm comprises of two electrical processes, impulse formation and impulse conduction.


 0 kommentar(er)
0 kommentar(er)
